Oestrogen–Gut Microbiome Axis: Physiological and Clinical Implications
Within each human gastrointestinal tract there is an exclusive combination of different communities of organisms, including bacteria, viruses, archaea, protozoa and fungi, which are collectively referred to as the gut microbiota and outnumber the total amount of human cells in the human body. The collection of these microorganisms, their genomes and the factors they produce are all part of the gut microbiome.The composition of the microbiome in the gut

Microbiome – an extra organ?
Increasing evidence suggests that these microorganisms actively participate in shaping and maintaining our physiology almost as an extra organ. Gut microbiota composition is associated with many health benefits, including maintenance of intestinal homoeostasis, protection against pathogens, and appropriate immune responses. Conversely, many gastrointestinal disorders such as irritable bowel syndrome and inflammatory bowel disease are associated with an imbalance in this microbial population. Furthermore, differences in diversity and composition of the microbiota have been linked to extra-intestinal diseases ranging from obesity and asthma to a variety of brain disorders.
The gut microbiota helps break down food, and in doing so produces metabolites that can directly influence the physiology of host cells, including brain cells. Moreover, immune responses to pathogenic bacteria produce cytokines and lymphokines that can affect brain physiology. As the nervous system is a master regulator of host function, this allows microbes to influence a broad range of complex physiological processes. An improved mechanistic understanding of how bacterial molecules act on the nervous system could yield improved therapeutics for treating behavioural and neurological disorders.
The stability of the microbiome
The human gut microbiota is usually stable and resilient to transient perturbations. However, microbial composition or activity of the gut can be modified by variety of factors, including internal factors such as hormonal changes, or external factors such as diet, antibiotics, and stress.
The Microbiome throughout life



Physiological role of estrogen
The role of estrogens in female reproductive development and maintenance is well defined. In the lower female reproductive tract estrogen regulates this microenvironment through mechanisms involving increasing epithelial thickness, increasing glycogen levels, increasing mucus secretion and indirectly by decreasing vaginal pH through promotion of lactobacilli abundance and lactic acid production. Phytoestrogens have been shown to have the opposite effect on the female reproductive tract compared to estrogen. Mice able to produce the phytoestrogen, equol, have significantly thinner vaginal epithelia as well as lower uterine weight. However, the action of estrogen is not limited to reproductive tissues.
Oestrogen and the Gut
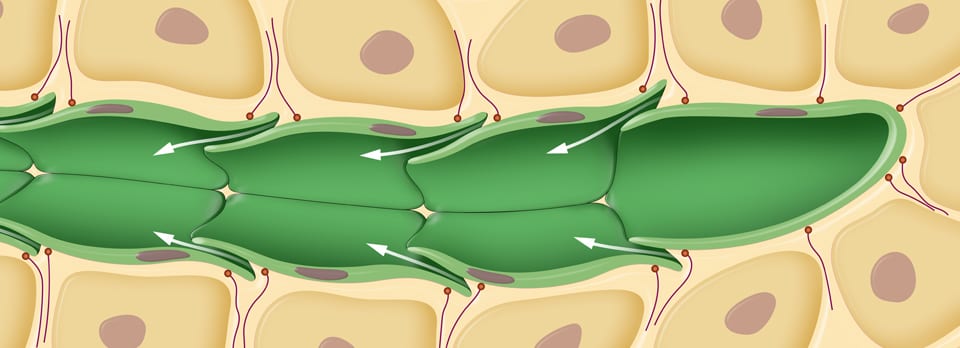
Gut epithelial barrier integrity can also be modified by estrogen. The dichotomy of gut epithelial integrity is illustrated through murine studies demonstrating that females are more resistant to gut injury compared to their male counterparts. Furthermore, it has been shown that that inhibition of androgens in male mice with flutamide results in reduced gut injury. A variety of tissues express estrogen receptors, including, intestine, brain, bone and adipose tissue.
As a result of this global expression, estrogen has been shown to influence a variety of physiological responses including neural development, cardiovascular health, bone density and neoplastic diseases including cancers.
During menopause a variety of negative health outcomes may occur from the depletion of circulating estrogen. This is a particularly important health issue as life expectancy continues to increase and the number of women ≥50 years old will increase by 60% between 2000 and 2025.
Sex hormones influence the gut microbiota
There is mounting evidence that steroid hormones can affect the gut microbiota. In support of steroids influencing the gut bacterial communities, sex differences have been noted in the composition of the gut microbiota with specific phyla, family and genera variances occurring with clear effects of gonadectomy and hormone replacement on gut bacteria in rodents. In mice, sex differences in the gut microbiota observed between males and females are decreased after castration, indicating a role for gonadal steroids in modulating the gut microbiota.
Administering testosterone propionate (1250 μg) to female rats on the day of birth decreased the diversity of the gut microbiota in adulthood by increasing the Firmicutes-Bacteroidetes ratio. This ratio increase may predispose the individual to obesity.
The gut can influence oestrogen levels
While gonadal steroids can alter the gut microbiota, it appears that, in turn, the gut microbiome can influence hormone levels. In postmenopausal women, gut microbiota diversity was positively associated with the ratio of estrogen metabolites in urine. In mice, transferring the gut microbiota of adult males to immature females caused an elevation in testosterone levels and metabolomic changes in recipient females. In addition, transfer of gut microbiota from male non-obese diabetic (NOD) mouse model of type 1 diabetes (T1D) to the female NOD T1D mice led to increased testosterone, metabolic changes, and protection against type 1 diabetes, which usually shows a strong female-to-male sex bias. These studies highlight the reciprocal connections between sex hormones and gut microbiota. Taken together, these studies provide strong evidence that the gut microbiota is influenced by gonadal steroid hormones and steroid levels can be altered by the gut microbiome.
Zearalenone makes ‘oestrogen’
Zearalenone (ZEA) is secondary metabolite synthesized by selected fungi of the genus Fusarium: Fusariumgraminearum, Fusariumculmorum, Fusariumcerealis, Fusariumequiseti, Fusarium-crookwellense, and Fusariumsemitectum (mostly F. graminearum and F. culmorum). ZEA is a non-steroidalestrogenic mycotoxin, chemically described as
Zearalenone exposure in human
ZEA is produced by fungi of the genus Fusarium, which attacks crops during its growth in the field as well as its time in storage. Humans can be exposed to ZEA directly by contaminated food or indirectly through products derived from animals exposed to mycotoxins. As it is not removed by the manufacturing process, ZEA affects the entire human food chain through a range of food products including cereals, meat, milk, wine, beer, dried fruits and spices. After ingestion, ZEA metabolites accumulate in various tissues (Brera et al., 2014). Moreover, ZEA might be also delivered with water contaminated with the fungus Fusarium Graminearum.
Zearalenone metabolism in human – it is not just oestrogen
ZEA, and its metabolites a-ZOL and a-ZOL, have an estrogenic effect associated with their structural similarity to estrogen. More-over, incubation with ZEA, a-ZOL and a-ZOL have been found to induce the production of progesterone, estradiol, testosterone and cortisol in an H295R cell line, indicating that not only ZEA, but also its metabolites, might act as endocrine-disrupting agents.
Estrobolome: Complex interplay between estrogen, the gut microbiome and distal mucosal sites
The ‘estrobolome’ is defined as the gene repertoire of the microbiota of the gut that are capable of metabolizing estrogens. Estrogens are metabolized by microbial secreted β-glucuronidase from their conjugate forms to their deconjugated forms. It is these “active” deconjugated and unbound estrogens that enter the bloodstream and subsequently act on estrogen receptor alpha (ERα) and estrogen receptor beta (ERβ).
Phytoestrogens are also metabolized in this manner, enabling their ability to act via mechanisms involving ERα and ERβ. Both estrogens and phytoestrogens can act genomically by binding to estrogen receptors, eliciting downstream gene activation and epigenetic effects and triggering of intracellular signalling cascades. This interaction leads to physiological changes across a variety of tissues ranging from neural development to reproductive health. Therefore, the gut microbiota regulates homeostasis at intestinal and distal mucosal sites. When dysbiosis occurs, these physiological responses are altered and contribute to disease states.
Oestrogen Dependent Cancers and Gut Microbiome
The novel implication of a recent study is that breast cancer was statistically significantly associated with other functions of the gut microbiota, unrelated to systemic estrogen levels. Low gut microbial diversity occurs with adiposity, insulin resistance, dyslipidemia, leukocytosis, and elevated C-reactive protein, some of which are associated with breast cancer.
How does the gut alter oestrogen levels?

The estrobolome and enterohepatic circulation of estrogens. Estrogens are primarily produced in the ovaries, adrenal glands, and adipose tissue and circulate in the bloodstream in free or protein-bound form and first undergo metabolism in the liver, where estrogens and their metabolites are conjugated. Conjugated estrogens are eliminated from the body by metabolic conversion to water-soluble molecules, which are excreted in urine or in bile into the feces. The conjugated estrogens excreted in the bile can be deconjugated by bacterial species in the gut with beta-glucuronidase activity (constituents of the ‘estrobolome’), subsequently leading to estrogen reabsorption into the circulation. Circulating estrogens exert effects on target tissues including breast, which stimulate cellular growth and proliferation. By modulating the enterohepatic circulation of estrogens, the estrobolome affects both the excretion and circulation of estrogens. In turn, the composition of the estrobolome can be shaped by factors such as antibiotics, other drugs, and diet that modulate its functional activity.
Conditions associated with the estrobolome: Endometriosis
Estrogen stimulates epithelial proliferation throughout the female reproductive tract and has been shown to drive proliferative diseases such as endometrial cancer, endometriosis and uterine fibroids. Endometriosis is common in premenopausal women, and coupled with its hyper-proliferative condition advocates that the disease may be mediated by high estrogen levels. Proliferation of endometrial tissue outside the uterus resulting in pelvic pain and infertility are hallmarks of endometriosis. Moreover, endometriosis can also result in menstrual disorders including menorrhagia. It is therefore promising that mediation of estrogen levels may alleviate hyper-proliferation associated with endometriosis. One caveat however is that other conditions can cause pelvic pain or ovarian cysts, thereby resulting in diagnostic dilemmas. For example, it may be confused with irritable bowel syndrome (IBS), since it too causes diarrhea, constipation and abdominal cramping.
Furthermore, IBS can accompany endometriosis, making it even more complex to diagnose. Gut microbiota shifts (lower lactobacilli concentrations and higher Gram-negative bacteria levels) have been demonstrated in a primate study of endometriosis, although the mechanisms linking these remain unclear. Gonadotropin releasing hormone agonist (GnRHa) stimulates the production of follicle-stimulating hormone and luteinizing hormone thereby suppressing estrogen production making it a common treatment for the estrogen-driven disease, endometriosis. Interestingly, GnRHa has been shown to impact the local microbiota of the uterus demonstrating the ability of hormonal regulation to modulate microbiota composition. Data elucidating β-glucuronidase activity in the gut microbiota of endometriosis patients may provide mechanistic insights into the role the estrobolome plays in endometriosis. The gut microbiome in patients with endometriosis may have a large number of β-glucuronidase producing bacteria which may lead to increased levels of estrogen metabolites and therefore drive endometriosis.
Polycystic Ovary Syndrome
Polycystic Ovary Syndrome (PCOS) patients have an increased incidence of metabolic syndrome, however, this incidence is not uniform across women from different countries and of varying ethnicity. PCOS is a hyperandrogen and low estrogen driven disease, and patients suffering from PCOS have significantly lower gut microbiota diversity compared to healthy controls. These variations in gut microbiome compositions highlight the interaction between microbiome composition, sex hormone levels and PCOS. Gut microbiome transfer from adult male mice to immature female mice has been shown to alter the microbiota resulting in increased levels of testosterone and to provide protection against type I diabetes.
The microbiome can increase testosterone
Testosterone has been shown to be produced in the gut by Clostridium scindens. Evidence of an increase in testosterone levels due to gut microbiome transfer coupled with direct evidence of testosterone synthesis from bacteria that inhabit the gut alludes to the existence of the “testrobolome”. Similar to the estrobolome, the testrobolome may influence sex hormone driven disease states that lack a clear link to estrogen such as PCOS.
Endometrial Hyperplasia
High levels of estrogen relative to progesterone can be found as a result of diseases such as PCOS and obesity. For example, the increased amount of adipose tissue in obesity results in the increased level of estrone conversion. This is particularly relevant in obese postmenopausal women for whom their major source of estrogen is adipose tissue. Increased estrogen production due to the high levels of adipose tissue is thought to be a key driver in female reproductive cancers and therefore hyperplasia. This idea is supported by the fact that female reproductive tract cancers are more prevalent in obese women. It is the reduction of progesterone levels relative to estrogen levels that is the principal driver of endometrial hyperplasia (EH) due to the lack of progesterone to oppose estrogen.
Increased estrogen levels as a result of estrogen-only hormone therapy results in an increased risk of developing EH. Much like PCOS, the risk of developing EH has been shown to be reduced following bariatric surgery. As previously alluded to in this review, bariatric surgery significantly alters both the microbiome composition and metabolic profile of obese women. Therefore, it may be the shift in the microbiome and metabolome composition as a result of bariatric surgery that plays a role in the reduced incidence of EH. The modulation of the estrobolome composition following bariatric surgery is a plausible driver in reduced risk of developing EH considering the critical role estrogen plays in driving the disease.
Infertility
Obesity has been shown to reduce spontaneous pregnancy rates and is associated with other obstetric complications such as preterm birth. Following bariatric surgery in obese women, fertility is improved and women with PCOS, a disease strongly associated with infertility, exhibit reduced symptoms. However, the metabolic aspects of PCOS are not restricted to obese women. Nonobese women with PCOS retain several hallmarks of metabolic syndrome such as insulin resistance, hypertension and increased risk of cardiovascular disease (CVD). This demonstrates that the alleviation of hallmark symptoms of PCOS is not simply mediated through weight loss, but rather through the modulation of the metabolic, including hormonal, aspects of PCOS perhaps through alterations in gut microbiota composition.
PCOS patients have an altered hormonal profile, which results in a dysfunctional menstrual cycle that ultimately leads to infertility. The gut microbiome composition is altered following bariatric surgery and that may be the driving factor that increases fertility and resolution of PCOS. There is an increase in circulating bile acids following bariatric surgery, which may be a direct consequence of the shift in microbiota composition. It is possible that a shift in microbiota composition that resolves PCOS also reduces a women’s risk of developing another infertility-linked pathology: endometrial hyperplasia (EH), following bariatric surgery. Fecal transplantation from healthy rats to a rat PCOS model as well as lactobacilli transplantation has been shown to improve estrous cycles and decrease androgen biosynthesis (a key component of PCOS).
PCOS has also been shown to be resolved through administration of metformin and clomiphene. Metformin and clomiphene are used in treatment of type II diabetes and in regulation of estrogen respectively. Metformin is now used to help treat the lack of glycemic control found in PCOS patients, which subsequently improves PCOS-associated infertility. Metformin has been shown to alter the gut microbiome composition, increasing Akkermansia spp. Abundance. Clearly, a complex interaction exists between the disease states which impact fertility and gut microbiota composition.
Oestrogen in the gut summary:
Made by
- Firmicute: bacteroidetes
- Reduced diversity
Stimulates
- biofilm
- Candida species (stimulates growth and morphogenesis)
- Coccidiodies immitis
- Chlamydia trachomatis
- Bacteroides melaninogenicus
- Pseudomonas aeruginosa
- Trichomonas vaginalis parasite
Decreases
- Staph aureus
- Sacchoramyces cerevisiae
- Paracoccidiodes brasiliensis
- Pneumococcal
- trichophyton
Testosterone
Made by
-
clostridium
Stimulates
- Streptococcus pneumoniaea
- Cocciodes immitis
Decreases
- Staphylococcus aureas
- S. epidermidis
- Strep faecalis
- Listeria monocytogenes
- Candida albicans
- bacillus subtilis
- micrococcus conglomeratus
- gaffkya tetregena
- bacillus cereus
- sacchoramyces cerevisiae
- Trichophyton purpureum
- Trichomonas vaginalis
Excess vitamin K2 supplementation makes biofilm. New target for future antimicrobial drugs
Cortisol by immune suppression allows stuff to happen but stimulates growth of bugs that cause periodontal disease.
Bugs Utilise Oestrogen
Fungi also utilize hormones (sometimes called pheromones) as messenger molecules that regulate various activities of the organism. Primarily, these molecules are related to control of sexual reproduction in various fungi, and take the form of novel steroids, peptides, and acid derivatives. In addition, fungi produce secondary metabolites, such as zearalenone, which has high estrogenic activity in mammalian cells. Zearalenone, and its metabolites, α-zearalanol, β-zearalanol, α-zearalenol, and β-zearalenol, act as a trigger factor for the development of central precocious puberty and high growth rate of girls exposed to environmental sources of these mycotoxins.
It has long been known that fungi can metabolize, transform and convert mammalian steroids (including the production of steroid molecules that mammalian cells cannot produce), which has proven useful in the biotechnology production field.
Oestrogen as a Pheromone
Estrogen works as pheromone and chemoattractant for candida to increase mating. A reciprocal mating pheromone system has been described in the human pathogen Candida albicans. Naturally occurring a and α clinical isolates have been identified and can undergo mating.
ZEA is produced by fungi of the genus Fusarium, which attacks crops during its growth in the field as well as its time in storage. Humans can be exposed to ZEA directly by contaminated food or indirectly through products derived from animals exposed to mycotoxins. As it is not removed by the manufacturing process, ZEA affects the entire human food chain through a range of food products including cereals, meat, milk, wine, beer, dried fruits and spices.
After ingestion, ZEA metabolites accumulate in various tissues. Moreover, ZEA might be also delivered with water contaminated with the fungus Fusarium Graminearum.
The take home message
There has been an explosion of gut research in the last few years that has shed light into the workings of the human body and more specifically the gut. With regards to the interaction of oestrogen and the gut we now know that oestrogen direct affects the gut microbiome and the microbiome directly affects oestrogen levels. Thus, if you have a cranky gut microbiome, this could severely affect your hormone levels.
We know from animal studies that transplanting ‘good’ bugs into diseased animals with PCOS helps improves their hormonal profile. This is ground breaking research and unheard of and unimaginable only a few years ago. Also, drugs like Metformin may exert their beneficial effects (or at least in part) via the gut.
So, the take home message is look after your gut because Hippocrates was right when he said the root of disease is in the gut.
References
Tetel MJ1, de Vries GJ2, Melcangi RC3, Panzica G4, O'Mahony SM5. J Neuroendocrinol. 2017 Oct 12. Steroids, Stress, and the Gut Microbiome-Brain Axis.Baker JM1, Al-Nakkash L2, Herbst-Kralovetz MM3. Maturitas. 2017 Sep;103:45-53. Estrogen-gut microbiome axis: Physiological and clinical implications.
Tetel MJ1, de Vries GJ2, Melcangi RC3, Panzica G4, O'Mahony SM5. J Neuroendocrinol. 2017 Oct 12. Steroids, Stress, and the Gut Microbiome-Brain Axis.
Tetel MJ1, de Vries GJ2, Melcangi RC3, Panzica G4, O'Mahony SM5. J Neuroendocrinol. 2017 Oct 12. Steroids, Stress, and the Gut Microbiome-Brain Axis.
Zearalenone as an endocrine disruptor in humans. Karolina Kowalska1, Dominika Ewa Habrowska-Górczyn´ ska, Agnieszka Wanda Piastowska-Ciesielska Environmental Toxicology and Pharmacology 48 (2016) 141–149
Zearalenone as an endocrine disruptor in humans. Karolina Kowalska1, Dominika Ewa Habrowska-Górczyn´ ska, Agnieszka Wanda Piastowska-Ciesielska Environmental Toxicology and Pharmacology 48 (2016) 141–149
Zearalenone as an endocrine disruptor in humans. Karolina Kowalska1, Dominika Ewa Habrowska-Górczyn´ ska, Agnieszka Wanda Piastowska-Ciesielska Environmental Toxicology and Pharmacology 48 (2016) 141–149
Kwa M1, Plottel CS1, Blaser MJ1, Adams S1. J Natl Cancer Inst. 2016 Apr 22;108(8). The Intestinal Microbiome and Estrogen Receptor-Positive Female Breast Cancer.
Plottel SC, Blaser MJ. Microbiome and malignancy. Cell Host Microbe. 2011;10(4):324-335.
Baker JM1, Al-Nakkash L2, Herbst-Kralovetz MM3. Maturitas. 2017 Sep;103:45-53. Estrogen-gut microbiome axis: Physiological and clinical implications.
Baker JM1, Al-Nakkash L2, Herbst-Kralovetz MM3. Maturitas. 2017 Sep;103:45-53. Estrogen-gut microbiome axis: Physiological and clinical implications.
Baker JM1, Al-Nakkash L2, Herbst-Kralovetz MM3. Maturitas. 2017 Sep;103:45-53. Estrogen-gut microbiome axis: Physiological and clinical implications.
Zearalenone as an endocrine disruptor in humans. Karolina Kowalska1, Dominika Ewa Habrowska-Górczyn´ ska, Agnieszka Wanda Piastowska-Ciesielska Environmental Toxicology and Pharmacology 48 (2016) 141–149
Zearalenone as an endocrine disruptor in humans. Karolina Kowalska1, Dominika Ewa Habrowska-Górczyn´ ska, Agnieszka Wanda Piastowska-Ciesielska Environmental Toxicology and Pharmacology 48 (2016) 141–149
Zearalenone as an endocrine disruptor in humans. Karolina Kowalska1, Dominika Ewa Habrowska-Górczyn´ ska, Agnieszka Wanda Piastowska-Ciesielska Environmental Toxicology and Pharmacology 48 (2016) 141–149
Zearalenone as an endocrine disruptor in humans. Karolina Kowalska1, Dominika Ewa Habrowska-Górczyn´ ska, Agnieszka Wanda Piastowska-Ciesielska Environmental Toxicology and Pharmacology 48 (2016) 141–149